
Sickle cell solution: Guiding teens and young adults through a crucial care transition
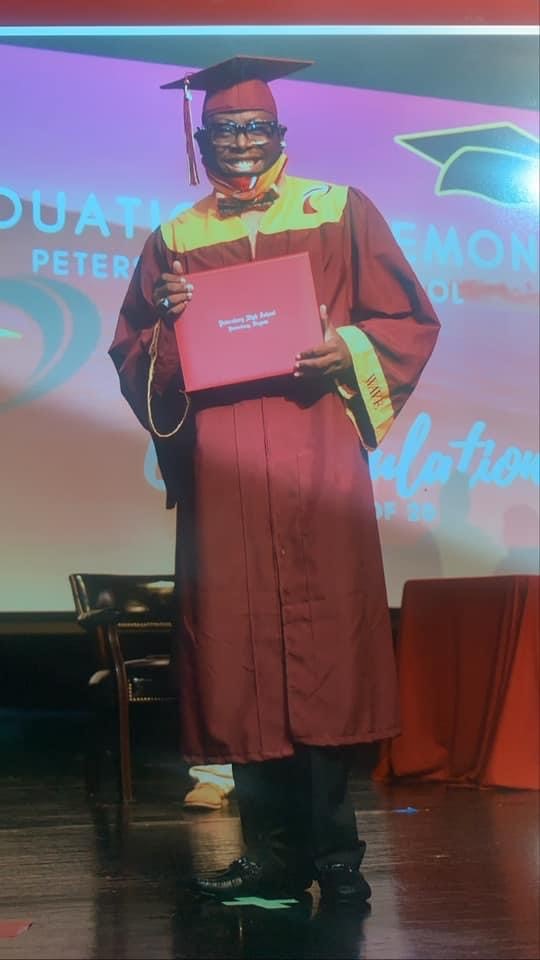
Sickle cell disease is unpredictable. One minute a person can feel good – the next, they’re on the way to the ED in excruciating pain. The teen and young adult years can be especially tough, something 20-year-old Deonte Grandison-King knows all too well.
A disorder of the red blood cells that carry oxygen throughout the body, sickle cell can cause complications from head to toe. The most common one is severe pain. As kids get older, complications tend to become more serious and pronounced. Teens and young adults often experience more pain crises, a higher risk of stroke and more frequent trips to the emergency room than they did in their younger childhood years. All this occurs while they’re graduating from high school, thinking about college or vocations, and transitioning away from a pediatric medical team that’s become like family to seeing adult providers.
“I built a lot of connections with my doctors over the years. It was hard when I wasn’t able to see them as frequently because I started seeing adult doctors,” said Deonte.
Approximately 320 pediatric patients get care for sickle cell disease at CHoR – and nearly half have the most severe form, hemoglobin SS. For these kids, a medication called hydroxyurea is prescribed to prevent pain and acute chest syndrome – two common complications related to sickle cell that can be serious enough for hospitalization. One of the big challenges in the adolescent years is that patients don’t want to take medicine or be ‘different.’ It’s also essential that they stay hydrated and keep up with their routine preventative care, including screenings for stroke, eye exams, heart echocardiograms and other monitoring to prevent significant organ damage. Often, schoolwork, friends, sports and activities take priority.
Overcoming obstacles – a national leader in sickle cell care transition
 Recognizing this as a crucial period in patients’ lives, our team has developed a sickle cell transition program to provide much-needed education and support. Teens enter the program when they start high school and the first step is going through a toolkit with the sickle cell social worker. The toolkit assessment covers whether they know their specific type of sickle cell disease, details of their insurance plan and other important health information.
Recognizing this as a crucial period in patients’ lives, our team has developed a sickle cell transition program to provide much-needed education and support. Teens enter the program when they start high school and the first step is going through a toolkit with the sickle cell social worker. The toolkit assessment covers whether they know their specific type of sickle cell disease, details of their insurance plan and other important health information.
“The toolkit helps our team determine what patients understand well and where they may have educational, psychosocial, family and other needs we can address over the coming months and years. It’s a good way for us to have a finger on the pulse of each individual patient,” said Jennifer Newlin, physician assistant.
In addition to Newlin, the sickle cell team includes Dr. Nadirah El-Amin, Dr. India Sisler, social worker Alesha Lieser, and educational consultants Kristie Elrod and Alma Morgan. Each week, they meet as a team, discuss the high school patients on the schedule and make notes about what to cover in the appointments. Using a binder they’ve put together that covers essential information, they provide each patient with focused education specific to their needs.
Sickle cell care and support beyond the walls of the clinic
While important topics are covered in each clinic visit, some things are better addressed in a more relaxed environment. That’s why our sickle cell team started overnight retreats in the fall of 2013 (with a brief pause during the pandemic). The retreats give patients an opportunity to meet peers who have grown up dealing with the same chronic illness.
“When we take our teens outside the clinical setting and they have a chance to interact with others who ‘get them,’ they become quick friends. It’s a safe place for them. Their medical team is here. We play games and try new things. It’s a really sweet time with the kids,” added Newlin. “Dr. Sisler and I are super competitive when it comes to games, especially spoons. Neither one of us likes to lose and the kids know it, so it’s always fun seeing who comes out on top.”
In addition to friendly competition, retreats at Camp Hanover have included dancing, skits, lip-syncing, scavenger hunts, fishing, canoeing, rock wall climbing and plenty of team building. Participants also talk about social/emotional concerns, goal setting and planning for the future. They share experiences, concerns, ideas and support.
Bridging the gap with a familiar face
Though Deonte’s schedule never allowed him to take part in the overnight retreats, he has appreciated another aspect of the transition program.
When Dr. El-Amin came on board in 2019, the team realized a new opportunity. Dr. El-Amin sees patients in both the pediatric and adult sickle cell clinics, bridging what can sometimes be a difficult gap.
“They allowed me to see Dr. El-Amin at CHoR first so I was in a safe space when I met her. Then, she asked me to see her in the adult clinic. It was a really good way to help me make the transition and Dr. El-Amin has been great about guiding me into this next chapter of life,” said Deonte.
Patients get to know the other members of the adult team, and vice versa, then care gradually transitions to new doctors who have gained an understanding of their history and needs.
“Moving from a team that has known and cared for you your whole life to new doctors and nurses can be hard. The hope is that by having a foot in both the pediatric and adult clinics, I can help make the transition a little smoother for our patients,” said Dr. El-Amin. “The pediatric and adult teams meet regularly to discuss patients who will be making the transition and develop a plan to for a smooth hand-off that meets their needs. We’re lucky to have a program where we can transition patients to adult providers in the same system. That’s very helpful for continuity of care – and not always the case at other hospitals and clinics.”
Collaboration across the country
While this system has been working great, the team never stops researching and seeking new ways to ensure the best care. Dr. Sisler is the principal investigator on a transition-based patient outcomes study currently in progress. The study involves centers across the nation, comparing the standard of care transition method (what’s being used at CHoR and VCU Health) with a peer mentor approach.
It’s also looking at the triad of pediatric care, adult care and support from community-based organizations – all of which play a role in helping patients in this critical stage. One of these community groups is Living with Sickle Cell, Inc., which is based in Richmond and has expanded to help more people virtually throughout COVID-19. The group allows participants to engage in discussion groups, monthly educational activities and mentorship relationships.
“The study is a collaborative approach to determining how we can best help our patients. In addition to looking at clinical and quality data, we’re engaging patients to see what they want and what would be helpful for them. As with most things in medicine, caring for teens and young adults with sickle cell disease is all about finding the balance between science and everyday life,” said Dr. Sisler.
As Deonte settles in with his new team, hundreds of teens will travel this path behind him – and benefit from the time, effort and care that continues to go into making sure each transition is a smooth one.
